Hi {{First Name|Timeless Autonomy Community}},
I hear from more and more healthcare providers and clinicians who are unsatisfied with their clinical careers.
It’s no secret that the healthcare workforce doesn’t have the long-term staying power it once did. Why?
Lack of autonomy
Heavy administrative burden
Lack of options for upward mobility
Unreasonable productivity requirements
Limited professional development opportunities
Salaries insufficient to cover the costs of repaying school loans
State licensing restrictions preventing work at the top of their license and scope of practice despite advanced degrees and board certifications
I have learned that clinicians are generally interested in a few areas where they think they can fit in healthcare organizations or health tech companies, like Product, Client Success, Sales, and UX design. Great options.
But what if the right early steps included first learning about the business and policy of healthcare and how you could make an impact? What might that lead to?
The first three areas I would focus on for professional development for healthcare professionals—physicians, APPs, nurses, PTs, OTs, STs, behavioral heath providers are:
Learn how health policy directly impacts professional behavior in healthcare delivery
Learn how incentives work in healthcare for providers all along the continuum of care and how different types of providers are paid
Develop a “capture habit,” and be able to synthesize information that resonates with you in a way that “your future self will thank you.”
Here’s what you shouldn’t do: go back to get another degree.
You may have just spent a fortune. You may be paying off debt.
You have a clinical license, something you have that others in Product, Client Success, Sales, UX Design, don’t have. Being a clinician is your superpower. Leverage it.
You can build the skills and knowledge you need through self-education.
Okay, okay, if you have your heart set on being a lawyer, accountant, or engineer, for example, that will require going back to school. They have different superpowers.
Made in Canva Pro
What I would focus on first? Understanding health policy.
Why? It’s something many others are intimidated by, it’s applicable to every role, it makes you more valuable to any employer in healthcare delivery or health tech.
To name a few reasons.
Make sure to get to the end of this post, where I share ways you can leverage health policy knowledge to grow your career as a healthcare professional!
One Resource to Bookmark
Kaiser Family Foundation (KFF) published this “Health Policy 101” piece that’s very readable. Dr. Drew Altman, the President and CEO of KFF, calls it a “mini textbook.” He also says this:
For us at KFF, our definition reflects our views and what we do: Health policy centers around, well policy–what the government does, and public programs like Medicare, Medicaid, and the ACA, and heavily emphasizes financing and coverage.
The resource ends with the Politics of Healthcare and the 2024 Election. You can find the resource here:
What actually IS health policy?
Health policy refers to the decisions, plans, and actions taken by governments, organizations, and institutions to achieve specific healthcare goals. These goals can range from improving overall public health to ensuring that everyone has access to necessary medical services.
Health policy involves figuring out how to allocate resources, such as money and medical supplies, and setting up rules and regulations to make sure these resources are used effectively. Well-designed health policy should create a system that helps people stay healthy and get the care they need when they are sick.

“Writing” by Notioly
In the United States, health policy covers many areas, including how healthcare services are organized and provided, health insurance, public health programs, and the regulation of drugs and medical devices. Policymakers aim to balance cost, quality, and access to ideally create a fair and effective healthcare system.
The Government Establishes Policy
Government programs have been established by laws passed by Congress and signed by Presidents, and regulatory bodies (In health policy, the Center for Medicare and Medicaid Services (CMS) and the Food and Drug Administration (FDA)) use the Notice and Comment Rulemaking (NCRM) process to define, refine, and update policy annually.).
Government health programs are part of mandatory federal spending, which means they must be funded through Congress fully every year. To make sure this happens, mandatory spending goes through the expedited Budget Reconciliation process. It’s supposed to be “clean,” meaning other bills and spending aren’t added, which could be barriers to the mandatory funding getting completed.
Graphic Designed in Canva Pro
Health Policy
I like to bucket healthcare delivery policy like this:
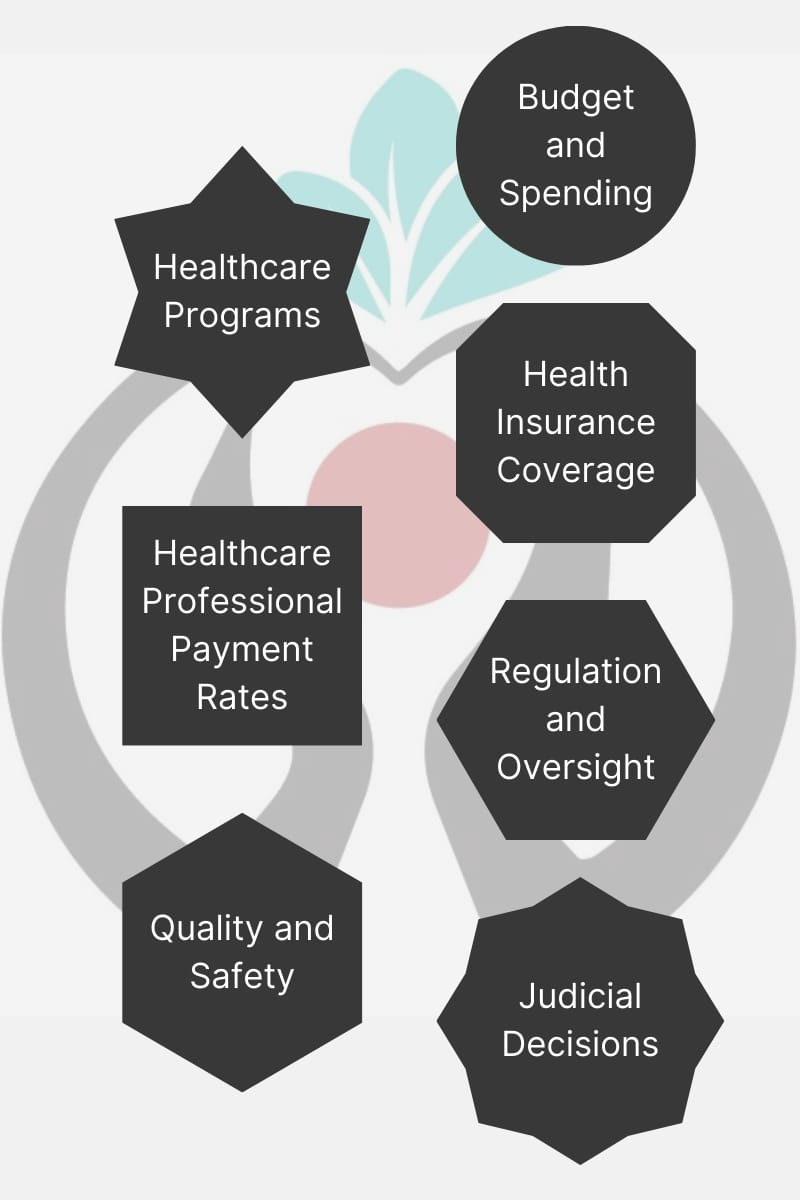
Designed in Canva Pro
Here’s a high-level overview of the Congressional budget and related rulemaking process:
As you know, Congress passes bills, and the President signs them into law. These laws establish and fund government programs, among other things. Medicare, Medicaid, the Children’s Health Insurance Program, the Affordable Care Act marketplace, and more are all established and then regulated through this process.
Next, regulators have to use their statutory authority, or authority provided by the law, to make annual “rules” for how a program signed into law is carried out and updated. In the case of healthcare delivery, we can use the Physician Fee Schedule as an example.
I’ll get into more detail on the 2025 Proposed Physician Fee Schedule in my next issue on “Incentives,” but here’s an example of what we find when we review a Proposed Rule.
It’s a “Proposed Rule” because the law states this regulation is updated through annual “Notice and Comment Rulemaking,” or "NCRM.” Once the Proposed Rule is issued, anyone can send comments on it on regulations.gov within 60 days. Those comments must all be reviewed and taken into consideration by regulators before the “Final Rule” is issued, which will create updates that go into effect sometime in the future (often the next or following year).
Rules can be changed by Congress. Before or after a Final Rule is published, stakeholders who don’t want to changes to go into effect can make their case to Members of Congress. Sometimes those requests end up in legislation (law) passed at the end of the year.
This year, like last year, CMS proposed some new services and codes for use in advanced primary care settings.
These are consistent with their goal of strengthening primary care, improving its funding, and incentivizing longitudinal, instead of transactional, patient care. Because these new codes are much easier to implement when used by participants in an accountable care organization or other alternative payment model, they also help CMS meet their 2030 goals. See CMS’ 2-page At-A-Glance on their Strategy Refresh, and the full document linked below:
So whatever federal funding CMS allocates in one area of a regulation has to be accounted for in others. The program is budget neutral and there are no increases for inflation built into the Physician Fee Schedule (PFS), another issue that may be addressed by Congress in the next few years. As many readers know, the PFS conversion factor has been reduced every year in the recent past. This is to account for increased utilization and billing by professionals who bill its codes.
Congress funds the whole PFS every year, and CMS decides how and where it will be allocated. One thing they have done in the last few years is add new billing codes for longitudinal patient care.
By adding codes for services often being done already but with no billing codes associated with them, they also assume providers will begin using these codes, leading to higher reimbursement to the practice. Examples finalized for 2024 were the Caregiver Training codes, Community Health Integration codes, and Principal Illness Integration codes.
These changes must be accounted for in other parts of the physician fee schedule. CMS adjusts the value of services billed by different healthcare professionals to account for new or more heavily-weighted services. The reason some providers will see a net negative or net positive impact from the budget and the change to the conversion factor is because of where funding was distributed.
So here’s where the influence of politics intersects with policies and regulations.
Using our example, CMS acts to boost funding and services in primary care, which aligns with the goals of President in office and its regulatory bodies. It’s also helpful to know that the top leaders (and others) in these bodies, like CMS, are appointed by the President, but many are “career regulators,” giving stability in rulemaking. Regulators are the subject matter experts in the federal government.
Congress receives feedback from interested parties and has the authority to stop the actions of regulators. They made place a “hold” on a new code that will shift spending away from one group and towards another.
The G2211 code is a great example of this. This is an “add-on” code for visit complexity. It was originally proposed in 2021 but delayed by Congress for three years, partly because of the impacts it would have on the weighting of reimbursements of some healthcare professionals who won’t be eligible to bill the code, like surgeons.
Congress received feedback from interested stakeholders and acted to hold on its rollout by CMS until 2024.
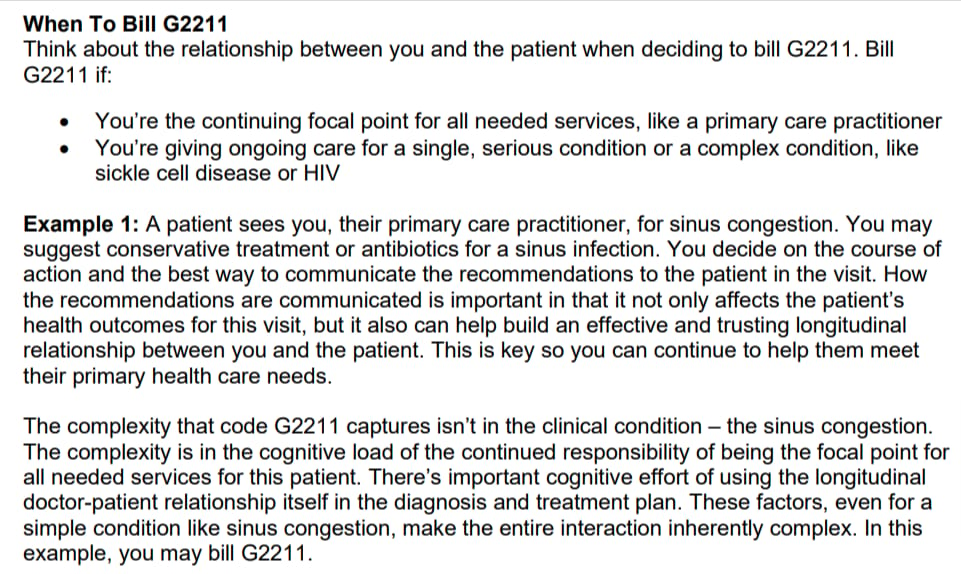
Here’s an example of when this G2211 code can be used, right from the above-linked MLN:
Here’s a Healthcare Dive article from September of 2023 about concerns that Congress could delay the implementation of the code again:
Understanding how Congress makes healthcare laws and how CMS regulates them is crucial for healthcare professionals looking for career growth and opportunities.
Health policy intersects with healthcare administration, the business of healthcare, health tech, politics, and more .
Here are the kinds of questions you are prepared to answer when you understand how health policy is developed, paid for, and regulated and follow developments in health policy.
How have health policies impacted telehealth services and what changes are permanent?
What is the role of health policy in addressing the opioid crisis? Which regulatory updates have removed barriers for those with substance use disorder from accessing treatment?
How do health policies influence emergency preparedness and response?
How can the safety of patients in skilled nursing facilities be influenced by federal policy?
How is CMS addressing maternal health through annual rulemaking and how should hospitals prepare for upcoming requirements?
What is the role of health policy in promoting healthy lifestyles?
What trends in federal home-based care policy are influencing changes to state laws?
How does CMS incentivize home-based peritoneal dialysis and other improvements to quality of care for ESRD beneficiaries in Innovation Center Models?
How do health policies impact disability services and support?
What can I do to influence health policy changes?
What are the current trends in health policy and how can I leverage them in strategic planning for my organization and for exploring career development opportunities?
How does health policy impact public health initiatives?
How are value-based payment models developed and evaluated?
How are pharmaceuticals and medical devices regulated?
What health policy changes could we expect in a change of party in the Executive Branch of the federal government?
How can healthcare innovation be facilitated or slowed by health policy changes?
How do regulators update rules to incentivize providers to create a safer healthcare experience for patients?
What is the relationship between health policy and health economics?
Which committees of jurisdiction in Congress develop and mark-up healthcare bills?
How can I work with others in developing and submitting health policy proposals?
How do international health policies compare to those in the U.S.?
What is the role of health information technology in health policy?
How does the Preventive Services Task Force for recommend services to be covered under Medicare without a copay?
How can I participate in advocacy to change or create health policy?
What regulations are at risk of being contested as a consequence of the Supreme Court overturning Chevron? How could this impact my employer and what could that mean for me?
Check out some ways you can leverage health policy knowledge for career growth as a healthcare professional!