In this Article:
Types of care in the home
Why is care moving into the home?
Alternative payment models that will drive more care into the home
Organizations driving care into the home
What does this mean for healthcare professionals?
Here is that list again:
Improved access and reduced barriers to care
One on one attention to patients, facilitating care of medical and non-medical drivers of health
Less exposure to pathogens for complex, multimorbid patients
Reduced likelihood of long episodes of care and their negative, long-lasting consequences
Avoidance of dangerous transitions of care
Moving care into the home is a shift that’s not only changing how care is delivered but also how it is paid for and who is delivering it. Let's explore that this entails, why this change is happening, and what it means for healthcare professionals.
Types of Care in the Home
Care in the home, or “home-based care,” encompasses a wide range of services that can be delivered in your home for illness or injury. It is often cheaper, more convenient, and just as effective as care you get in a hospital or skilled nursing facility.
But what do we mean when we say “care in the home” or “home-based care?”
If we go back about ten years ago, most of us in the healthcare industry would have described home-based care in two '“buckets”: professional home health services (generally billed under a payer’s hospital or Medicare Part A benefit), or custodial care (home health aide services).
Professional Home Health Services
This is a common pre- and post-acute medical benefit where, at minimum, registered nurses and/or physical therapists, after referral from a qualified practitioner (generally physicians, although there are waivers available in alternative payment models (APMs) for nurse practitioners and physician assistants to sign home health orders and related documentation).
In the case of Traditional Medicare (TM)/Medicare Fee-for-Service (FFS), Medicare reimburses a certified home health agency for 30-day episodes of care. A patient may be “recertified” for multiple episodes of care, as medically necessary.
The evaluation for home health (known as the OASIS for Medicare beneficiaries), must be conducted by a registered nurse (RN), physical therapist (PT), speech language pathologist (SLP), or, most recently added, an occupational therapist (OT). Orders can be requested and provided for a range of services after that visit, including medical social work (SW), registered dietician (RD), and supportive, short-term home health aides services (if a registered nurse is part of the care team).
The payment by TM, at a high-level, is an episodic-based payment essentially based on the responses to the OASIS evaluation and documentation form. The present payment system is called the “Patient-Driven Groupings Model,” or PDGM, for Medicare beneficiaries.
A patient qualifies if determined by their provider to likely have medically necessary skilled care needs provided intermittently (read NOT daily). The initiating visit can be provided in the absence of a hospital stay or after a hospital or inpatient post-acute stay (examples: inpatient rehabilitation facility (IRF) or skilled nursing facility (SNF)). Home health initiated after an inpatient stay is reimbursed at a higher rate under PDGM.
Patients must also meet “homebound requirements.” There are exceptions to this rule, such as when this is waived (upon application) as a flexibility in some advanced alternative payment models.
The primary barrier to more patients discharging from hospital to Home Health for their post-acute care is that the intermittent nature of home health requires caregiver support.
Here’s an excellent visual and linked article discussing this:
Custodial Home Care Services
This is short or long-term non-skilled care provided by certified home health aides (CHHAs). It may be necessary and/or beneficial for an episode (after an illness or injury to facilitate a safe, successful recovery) or become necessary on an ongoing basis for an individual to remain home safely and successfully.
Common home care services include personal care, activities of daily living support, feeding support, housekeeping support, laundry services, errands, etc.
How home care services by CHHAs are reimbursed depends on one’s healthcare payers.
Let me explain.
Custodial care is not medical care, even though it may be necessary to keep an individual home, mobile, well, and out of an inpatient facility to live (such as assisted living and skilled nursing facilities/LTC facilities). Only medical care is paid by medical insurance, like Medicare and Commercial payers.
However, for those who qualify for community Medicaid, they may be eligible for long term, in-home support, depending on the state in which they live. Medicaid home care services run the spectrum of coverage from a few hours per week to 40 hours per week and more.
Why does Medicaid cover this and Medicare does not?
For those who are dual-eligible for Medicare/Medicaid and for those with Medicaid as the primary payer, Medicaid will be obligated to pay for long term care in a skilled nursing facility.
Increasingly, Medicaid plans have crunched the numbers and more are willing to pay for community support at some level. The level of community Medicaid reimbursement will often be a major determining factor as to whether an individual must live out their lives in a facility or in their community residence.
In addition, Medicare Advantage (MA) regulations have evolved significantly over the past 5 plus years.
MA Special Needs Plans (SNPs) often cover home care services, as do Medicaid CMS Innovation Center models and dual MA/MCO integrated plans.
Healthcare at Home: What’s new?
Home Health and Home Care are two of many types of healthcare being provided in the home. Here are some others:
Primary Care at Home
To get to a doctor’s office, there are many steps and considerations that can be heavy lifts 🏋♀️for the frail, multi-morbid, and/or seriously ill individual. Here are some:
Shower, get dressed, brush teeth, do hair
Arrange a ride and someone to assist you
Manage your energy levels so you have the endurance to complete the event, focus
Remember to bring a list of things to talk to the provider about
Consider physical barriers and how you will manage them
Making sure someone can be with you to listen and ask questions, get up and down from a chair and the care, and to support you if you are are afraid of falling or off balance
Have portable oxygen ready and tanks full if you need them
Toileting concerns like incontinence
You can see how it’s easy to postpone, ignore, or give up on maintaining a relationship with an office-based provider. Our most vulnerable patients are the ones we most need to see and have the most barriers to see us.
Fee-for-service made home-based physician care almost obsolete. Medicare pays no more for home-based visits than office visits. The visits take longer, there is no one there to help like in a practice setting, and there is “windshield time.” A primary care provider who can bill 24 Relative Value Units (RVUs) in one day in an office might be able to bill 8-10 RVUs in home-based settings.
It’s easier for providers to visit patients living in group settings like assisted living facilities (ALFs) and SNFs, of course, and this is yet another reason why so many vulnerable patients eventually, often after failing to get the care they need at home to stay home, end up in a facility after deterioration, so they can get even more care.
CMS and the Innovation Center have developed alternative payment models through their statutory authority to address this issue. Models such as the Independence at Home model (IAH) and Program for All-Inclusive Care of the Elderly (PACE) shift incentives to address specific populations through care in the home.
Organizations like Bloom Healthcare provide in-home primary care and are reimbursed through fully at-risk Medicare Models. I wrote about their results in Direct Contracting here.
Urgent Care at Home
Complex patients also need access to urgent care before it becomes life-threatening and in the comfort of their own homes. While there are some reimbursement challenges in this setting, also, there are organizations doing this successfully.
To provide urgent care that includes most of what an ER would, visiting providers needs immediate access to tools like IV supplies, sutures supplies, medication, injections, and so much more. Providing urgent care (usually same day) requires different tools than those for a physician “sick visit.” It usually involves a provider and another support person (like an EMT), and extensive mobile supplies.
Two examples of urgent care at home types:
Private organizations like Dispatch Health. They offer a variety of services, depending on their location, but have been providing urgent care for many years. They sometimes partner with payers and/or at-risk providers who have incentives to reduce avoidable ER visits and hospital stays.
Paramedicine program. One alternative payment model that provided more flexibility for paramedics to treat onsite and avoid preventable ER visits was the Emergency Triage, Treat, and Transfer Model (ET3).
One of the challenges of the ET3 model was the variability in state regulations for paramedic scope of practice. Emergent, rapid response medical care in the field is provided by a wide variety of clinicians with a host of educational backgrounds. There is untapped potential to optimize emergency service resources, but the variability in scope per state and per license type, as well as the resources devoted to preventing “scope creep” of non-physicians by the American Medical Association are limiting factors in harnessing this potential. Hence ET3 was ended two years early.
Outpatient Physical Therapy at Home
Forward-thinking physical therapist entrepreneurs have created solutions to address the inconvenience and sometimes impractical nature of managing patients in a PT clinic. Those with balance issues, medical frailty, transportation limitations, impaired mobility, and much more are better suited to being treated at home.
While home health under Medicare A covers PT at home, there are guardrails that limit who can be admitted and for what purpose(s), while the regulatory and payer “bars” for treating under the outpatient benefit in PT (and OT, ST) are aligned with the outpatient setting.
PTs practice under general supervision in Medicare and under “direct access” licensure in all states (some with full direct access, others with some). Payers vary in coverage without physician prescription, but the relationship between the cost of physical therapy and downstream savings impacts are incentivized by VBC arrangements.
Luna Physical Therapy is doing this very well. Some snips from their website:

I expect the need for in-home therapy to grow with the rollout of the GUIDE Dementia Care Model, also. I wrote about GUIDE here. Hospital at Home, which is likely to be extended by Congress before it expires on December 31, 2024, needs PTs to go to the home. And then there’s “SNF at Home,” another program type in development to facilitate recovery in the home setting, rather than inpatient settings.
Hospital at Home
Hospital at Home has been part of value-based care contracting for a number of years. But it’s gaining popularity since the COVID PHE and the CMS waiver, which was extended for two years and is likely to be extended further, as the initial evaluation of outcomes was positive in quality and spending.
Bruce Leff, largely considered the father of Hospital at Home, co-authored this article in Health Affairs last Month (May 3, 2024). He authored this article, where he states Hospital at Home is the cornerstone of the future home-based care ecosystem.
Post-Acute Care at Home/SNF at Home:
Another type of care that is ripe for home-based innovation is an alternative to skilled nursing care at home. Again, there is some innovation here in value-based contracting, but there is not yet a Medicare Fee-for-Service program.
As noted above, the primary barrier to patient’s returning home after a hospital stay is the amount of support at home by family caregivers. While the clinical support in home health is high, successful recovery often depends on the support and education of family caregivers.
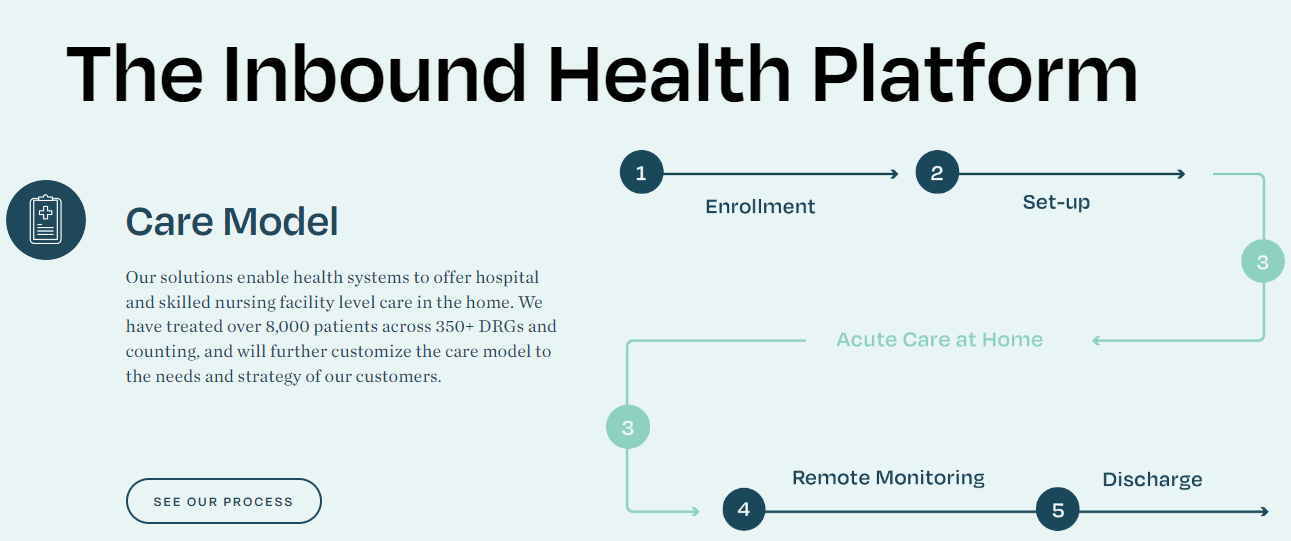
One innovator in this space is Inbound Health.
From Inbound Health’s website:
Personalized care plans may include in-person nursing and therapy visits, daily virtual visits with our hospitalists and SNFists, mobile labs and imaging, home-based equipment, medication consultation and administration, non-emergency transportation, and more. All the while, the patient is monitored 24/7 by our clinical command center leveraging biometrics and digital surveillance coming from our proprietary digital engagement platform.
Throughout their stay, the clinical care team is just one click away. Our team leverages predictive analytics to ensure the patient’s care journey is customized to meet the patient’s medical and functional complexity. If a problem or need arises, our high-touch model allows for instant digital or in-person engagement and teams are rapidly deployed to the patient as necessary.
Skilled nursing at home (or whatever it ends up being called) can also serve the role of a transitional site of care with in person and remote physician and advance practice provider visits for patients who need a short period of close medical oversight in addition to custodial support, rehabilitation, and nursing care.
Concurrent Care for Hospice Beneficiaries
In the Medicare Care Choices Model (MCCM), CMMI tested a option for hospice agencies to participate in a model targeting hospice-qualifying beneficiaries who didn’t want to opt into the full hospice benefit (which requires curative treatment end). The MCCM option was often an on-ramp to hospice and the results were remarkable. Read more about the model, its results, and options available to mirror MCCM here:
Home Dialysis for End Stage Renal Disease Patients
Some of the most complex and high-cost patients are those with end-stage renal disease who must rely on dialysis as a lifeline. In-home dialysis is an option being incentivized through new Innovation Center Models in the kidney care space.
One example is the Kidney Care Choices (KCC) Model, with 99 present participants. Some organizations providing services to or enabling care for the ESRD population:
This is not an exhaustive list of health care at home types.
It doesn’t touch on the technology enabling in-home care, for example, or where policy is headed and how it may be funded and regulated long-term. That’s a topic for another article.
In the meantime, here are two of my favorite “go-to” resources on telehealth/telemonitoring health policy:
What does all this mean for healthcare professionals?
The business and practice of in-home healthcare delivery, technology, public policy, payment reform, alternative payment models, and more…
…is changing, growing, and becoming more popular with consumers.
Innovative entrepreneurs and investment firms are devoting time and money into this space while it’s still “early.”
Home-based care innovation has accelerated since the COVID pandemic.
Healthcare consumers want to see more of it.
Baby boomers want to age in place.
Payers are funding more of it.
Technology is enabling it.
Policy is facilitating it.
Expect more growth.
Learn more.
Additional reading: